Terry O’Neill has devoted much of his career as a journalist to writing, editing, and assigning stories about euthanasia and abortion. As a journalist, O’Neill has committed himself to the pursuit of truth.
He left journalism a dozen years ago to pursue another line of public service: municipal politics. But just over five years ago he retired from the political life and returned to journalism, contributing to The B.C. Catholic. Since then he has been digging deep into the depths of the MAiD crisis, shedding light on the rising concerns about a system gone fatally off the rails, particularly in British Columbia.
In that time, O’Neill’s reporting has been recognized with numerous awards from Christian and Catholic media organizations in the U.S. and Canada.
As part of this special section devoted to Canada’s euthanasia crisis, we review below some of the B.C. Catholic’s coverage showing how badly the euphemism Medical Assistance in Dying, or MAiD, has corrupted the medical system and how urgently reform is needed.
MAiD became law in 2016, and it was supposed to be only for those facing imminent death and who were in unmanageable pain. Then, of course, eligibility was greatly widened in 2021 to include, basically, anyone who had given up on life.
But even before that court-ordered expansion, O’Neill started hearing stories emanating from hospitals and hospices within the Fraser Health Authority region—the largest health authority in British Columbia.
In early March 2020, O’Neill filed a Freedom of Information request, asking to see all reports and studies dealing with the preparation and implementation of the Fraser Health Authority’s MAiD program. He wanted to know if there was anything in writing instructing doctors and nurses to encourage MAiD.
Then COVID hit, and it took him a year to finally get his answer. No. All the material he found in the heavily redacted documents said MAiD was to be a patient-led process.

O’Neill found an apparent contradiction. The process was clearly not patient-led. Patients felt pestered, badgered, and asked to sense that they were encouraged, yet no one was being held accountable. No one was explaining the contradiction. It was all a big lie, and people weren’t supposed to question it.
At the same time, O’Neill was learning that patients were being allowed to have themselves killed, even though they didn’t appear to meet the then-more-rigorous bar of being near death and being in unbearable pain.
O’Neill told the story of Alan Nichols, who was granted his death wish even though he was not dying. His brother Gary was aghast and told O’Neill, “my whole problem with MAiD is that the government opened the door to it, and doctors and others just opened it wider, with no accountability.” This was the slippery slope.

O’Neill wondered what the redacted parts of the Fraser Health document—including reports, agendas, and minutes of in-camera/closed-door meetings—said about all this, so he filed an appeal in an attempt to pry open those secret documents.
While he awaited the outcome of that appeal, more and more people contacted him to talk about their concerns.
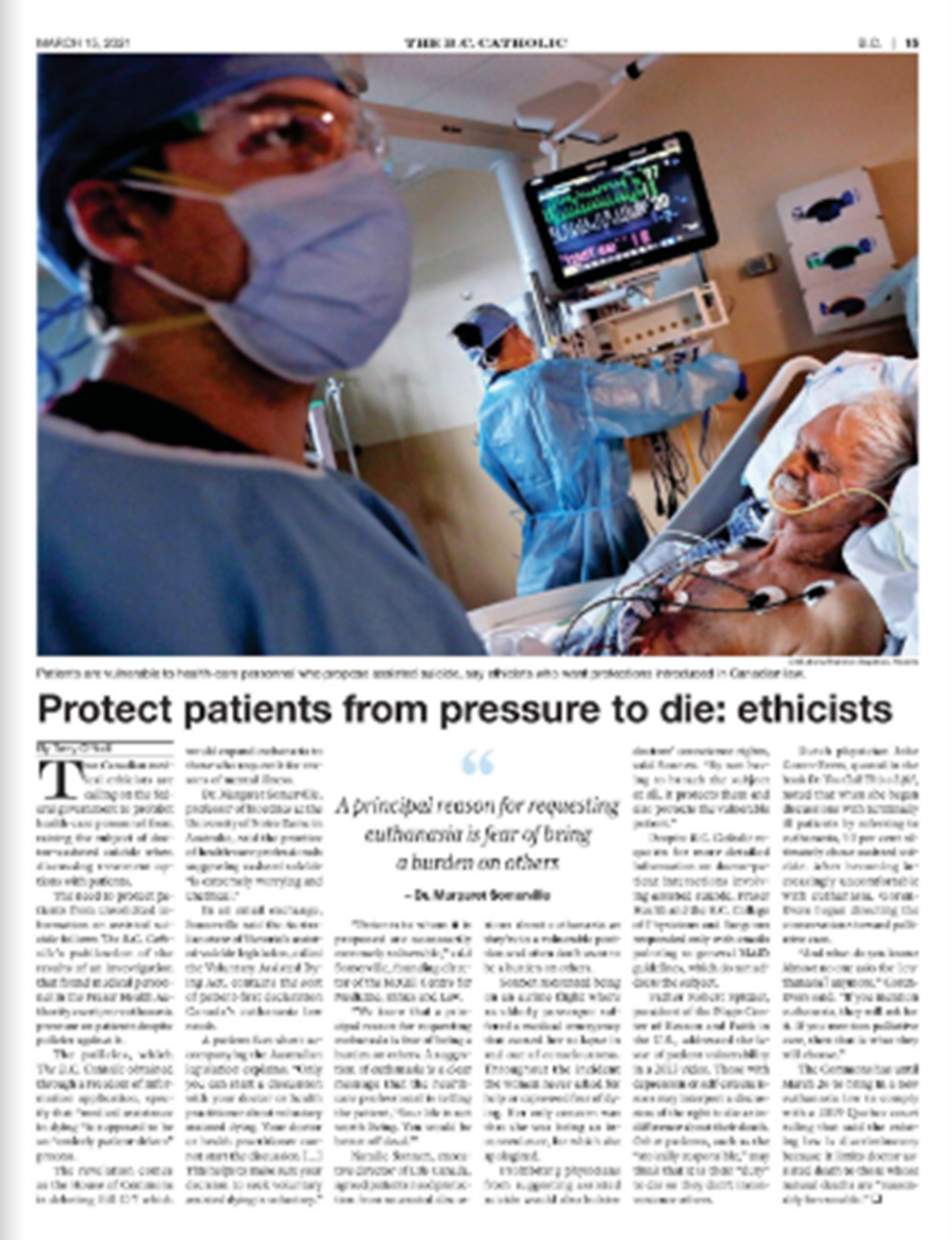
In a story he published just two weeks after the Nichols story, O’Neill reported that a group of Canadian medical ethicists were imploring governments to prohibit medical personnel from being the first to raise the subject of MAiD when meeting with patients. It turns out that doctors were raising the subject of MAiD as part of an information package about “possible courses of action” (like intensive treatment, palliative care, etc.)—as if obliterating a person’s life were the same as a course of radiation.
The ethicists were concerned many elderly patients are not only very vulnerable but also of the mind that they don’t want to be a burden. And so, when someone in authority suggests MAiD, the patients might think it is their duty to comply. O’Neill’s story also disclosed that the Australian state of Victoria explicitly prohibits medical personnel from raising the subject of euthanasia for this very reason.

The moniker “patient-led” can be misleading. In practice, doctors sometimes pressure individuals to make the decision, as illustrated in a story about a husband who was encouraged to euthanize his ailing wife.
And remember, with Fraser Health’s official policy being that MAiD must be patient-led, one would have thought that a similar prohibition would be in place here, too. But no.
O’Neill began to understand then why MAiD’s death count in B.C. was so worrisomely high. In a July 2021 story, O’Neill’s friend Alex Schadenberg, head of the Euthanasia Prevention Coalition, said another reason is that there’s no effective oversight of the doctors who authorize MAiD.
In the same issue that O’Neill wrote about the frighteningly high death toll, he reported on the case of an elderly Surrey woman, Joan Rohoway, who was nearing death and was losing her decision-making capacity when she was approached by a Fraser Health team and talked into allowing herself to be killed. That’s her picture on the right, with her family. But before that could happen, her anguished daughter and son-in-law raised bloody hell with authorities and had the procedure stopped.
O’Neill spent several hours visiting with the family and had a short conversation with Joan, who said simply, “I want to live.” Just a few weeks later, she died naturally, with her family at her side. May she rest in peace.

O’Neill’s next major article centred around Fraser Health’s surprise, last-minute decision to release some of the secret documents it had earlier withheld. So, in late November 2021, O’Neill published a story detailing the secret deliberations that saw the Fraser Health board reject out of hand the reports of its own palliative care experts, urging the board not to order that MAiD be thrust into every Fraser Health facility, including hospices and palliative-care wards. To do so, the experts argued, would destroy palliative care.
O’Neill paused for a moment to honour and acknowledge Dr. Neil Hilliard, who was the respected head of palliative care for the Fraser Health Authority region in 2017 when a board-mandated policy, calling for FHA leadership to support the provision of doctor-assisted death in palliative-care wards and hospices, forced him to resign on a matter of principle.
Dr. Hilliard had led the charge to oppose MAiD in palliative-care settings, arguing its focus on so-called medical death would seriously injure authentic palliative care by draining resources and changing staff focus.
Dr. Hilliard told O’Neill that, after he read the heretofore-secret Fraser Health Board minutes that O’Neill showed him, he wondered why all of this had to be discussed in-camera and then was originally redacted. “Was this to prevent opposition to the agenda to provide MAiD ‘wherever the patient resided’ under the guise of patient-centred care? Was the palliative-care program now considered the enemy because of its philosophy to help people with life-limiting illness live well until they die a natural death?”

He also said for the 95 per cent or more of individuals who do not choose MAiD at the end of life, do in-camera sessions and redacted minutes inspire trust in the health authority? Do bullying tactics against hospices, which wished to stay true to their founding principles of palliative care, inspire trust? If the palliative-care leadership does not have freedom of conscience to provide palliative care, free from the provision of MAiD, or resign, how is the rest of the palliative-care team to preserve its own integrity?
He told O’Neill one can see from the minutes that, from the very first, there was a bias to MAiD. The truth is that the provision of MAiD is the antithesis of palliative care and should not be merged but kept separate from palliative care. Deception is even present in the term “Medical Assistance in Dying,” since this is what palliative care has been all about from the beginning, but not by intentionally ending a patient’s life.
To regain trust in the provision of palliative care, Dr. Hilliard said “hospice sanctuary” will be necessary, funded privately and not subject to government- or health-authority-forced direction to provide MAiD. This, of course, is what Delta Hospice Society is aiming for.
Officials with the FHA did not answer O’Neill’s questions about why the board’s MAiD discussions took place in secret, why the FHA initially withheld release of the documents, and why they ultimately made the records public.
O’Neill’s stories continued throughout 2022, reporting for the first time anywhere, for example, how MAiD proponents were pressuring the B.C. government to force religious facilities, like the Catholic Providence Health Care authority in Metro Vancouver, to allow MAiD in their facilities. The issue came to a head a year later at St. Paul’s.
By now, other media outlets were covering MAiD outrages in Canada—how veterans of the Canadian Armed Forces were being offered MAiD instead of treatment, how the poor and the disabled were turning to MAiD because they couldn’t get adequate support under this country’s monolithic government-mandated medicare-care system. It was almost as if MAiD were being used to relieve the system of the pressure being built by so many poor souls being not able to obtain adequate care.
In May of 2022, O’Neill reported more about the adverse impact of MAiD on palliative care and how MAiD had become a cancer, eating away at the system. This story came after two of Canada’s leading palliative-care doctors testified to a parliamentary committee. O’Neill was particularly struck by one statement from Dr. Leonie Herx, who said that, as it now stands, Canadians have a legal right to medical assistance in dying, but not to medical assistance in living.
Polling of the public shows fairly strong support for MAiD, as long as the patient is dying, is close to death, and is truly suffering. On the other hand, though, polling shows growing concern for extending access to MAiD to those suffering from mental illness.
O’Neill reported on the controversy, and, as most people probably know, the federal government has now twice postponed its implementation. And the party currently leading in the polls says it will permanently shelve the plan should it be elected this coming fall.
And on and on it went. In December 2022, O’Neill told the story of Dr. Kevin Sclater, who quit his position at the Crossroads Hospice in Port Moody because, in part, of being forced to talk to patients about the availability of MAiD. One month later, Fraser Health—facing yet another FOI appeal that O’Neill filed—unredacted more documents that showed widespread staff opposition and concern over its cheerily enthusiastic embrace of MAiD.
A half a year later, O’Neill received more Fraser Health documents, revealing not much this time, but at the same time, he was contacted by two women who charged that medical officials at a Fraser Health facility had broken the law by euthanizing their mother under the auspices of MAiD because she wasn’t dying. Their complaint hit a dead end.

Last year, Paul Schratz wrote about the Fraser Health Authority sending its regional MAiD leader to give a presentation to a meeting of retired municipal employees in Surrey. Tammy Dyson met with members of the Municipal Pension Retirees Association in Surrey and delivered a PowerPoint presentation in which she explained MAiD eligibility criteria and the process for accessing assisted suicide.
When The B.C. Catholic contacted the health authority after the presentation, the authority said it doesn’t use methods such as presentations to share information with “patients.” But didn’t mention its practices involving non-patients.
And the stories continue to come, with controversies over allowing mature minors to access MAiD and allowing persons to sign advance directives for MAiD. O’Neill admits that he becomes cynical at times, thinking that if advance directives for MAiD become legal, we can take some comfort in the fact that waiting lists for medical services in Canada are so long that the MAiD-requesting person might die naturally while waiting to be killed unnaturally.
More recently, O’Neill has been writing about the provincial government forcing Providence Health to allow a MAiD facility to be opened next to St. Paul’s, to be run by Coast Health. He is currently investigating where the facility will be built and whether one will be mandated at the new St. Paul’s currently being built a few kilometres east of the existing one. So far the government is not responding to his questions.
MAiD’s rise in Canada came about because of Charter-based court orders. Interestingly, though, that same Charter gives Parliament or provincial governments the right to invoke the notwithstanding clause and then not implement MAiD.
O’Neill has repeatedly asked the leader of the most conservative of B.C.’s four main provincial political parties whether they might invoke the clause, or perhaps refuse to pay for MAiD procedures and/or MAiD drugs. It’s certainly within the province’s powers to do this. Each time he asks, however, the questions go unanswered.
Your voice matters! Join the conversation by submitting a Letter to the Editor here.